How can non-profit hospitals survive, and where does their funding come from?
Non-profit hospitals, cornerstones of community healthcare, face a persistent and multifaceted challenge: maintaining financial solvency while fulfilling their mission of providing care to all, regardless of ability to pay. Their survival hinges on a complex interplay of diversified funding streams, efficient management, and a constant adaptation to the evolving healthcare landscape. Understanding their funding sources and strategies for sustainability is crucial for both the institutions themselves and the communities they serve.
Unlike for-profit hospitals, non-profit hospitals reinvest any excess revenue back into the organization, furthering their charitable purpose. This means they cannot rely on shareholder dividends to bolster their finances. Instead, their financial health depends on a delicate balance of various revenue sources, each with its own limitations and vulnerabilities.
One of the primary sources of funding comes from patient revenue, encompassing payments from private insurance companies, government programs like Medicare and Medicaid, and out-of-pocket payments from patients. The reimbursement rates from these payers vary significantly. Private insurance generally offers the highest reimbursement rates, providing a crucial source of revenue. However, the increasing prevalence of high-deductible health plans and cost-conscious employers is putting pressure on these rates. Medicare, the government program for seniors and certain disabled individuals, reimburses at a lower rate than private insurance. Medicaid, the program for low-income individuals and families, typically provides the lowest reimbursement rates, often falling below the actual cost of providing care. This disparity creates a significant financial burden for non-profit hospitals, particularly those serving a large proportion of Medicaid patients. The Affordable Care Act (ACA) aimed to expand Medicaid coverage, which initially helped to alleviate some of this burden. However, ongoing challenges to the ACA and varying levels of state participation continue to create uncertainty and financial strain.

Philanthropy represents another vital, albeit often unpredictable, source of funding. Donations from individuals, foundations, and corporations can provide crucial support for capital projects, research initiatives, and uncompensated care. Developing strong relationships with donors and cultivating a culture of philanthropy are essential for non-profit hospitals. However, reliance solely on donations is unsustainable. Economic downturns can significantly impact philanthropic giving, leaving hospitals vulnerable. Therefore, hospitals must diversify their fundraising efforts and explore alternative revenue streams.
Government grants and subsidies offer another avenue for funding, particularly for specific programs or initiatives that address public health needs. These grants can support research, community outreach programs, and the provision of services to underserved populations. The availability of these grants is often subject to political priorities and budgetary constraints, making them an unreliable long-term funding source.
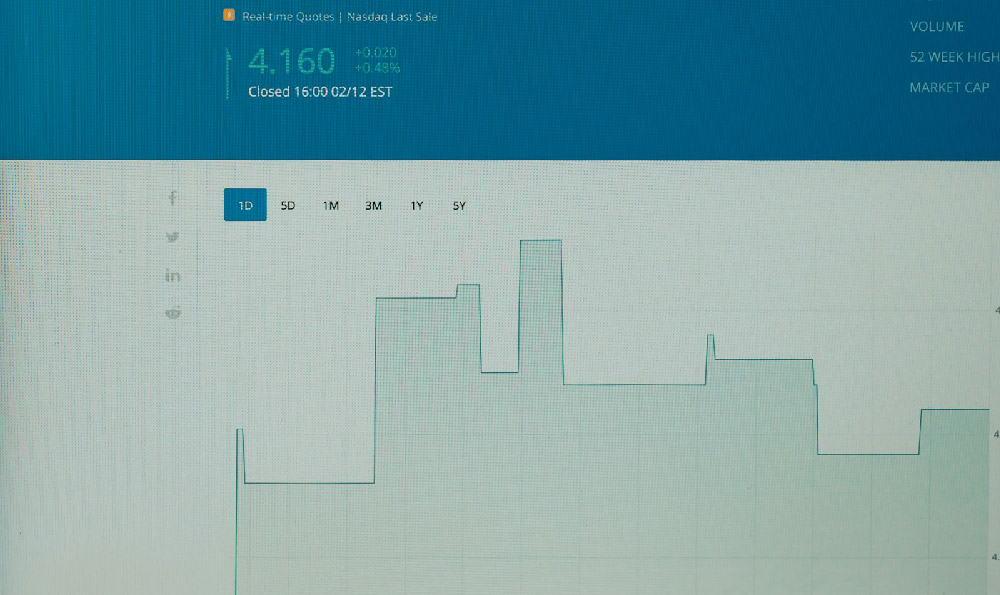
Investment income, derived from the hospital's endowment and other investments, can contribute to its financial stability. However, investment returns are subject to market fluctuations, and conservative investment strategies are often necessary to protect the endowment's principal.
To survive and thrive, non-profit hospitals must employ a range of strategies to enhance their financial performance and ensure long-term sustainability. These strategies include:
- Cost Management: Implementing rigorous cost-control measures is crucial. This involves streamlining operations, improving efficiency, and negotiating favorable contracts with suppliers. Hospitals are increasingly adopting lean management principles to eliminate waste and improve productivity. Supply chain management and group purchasing organizations can also help to reduce costs.
- Revenue Cycle Management: Optimizing the revenue cycle, from patient registration to claims submission and payment collection, is essential for maximizing revenue. This involves accurate coding, timely billing, and effective collection efforts. Investing in technology and training staff in revenue cycle best practices can significantly improve revenue capture.
- Service Diversification: Expanding services and developing new revenue streams can help to offset the financial pressures from declining reimbursement rates. This may involve offering specialized services, such as cancer care or cardiac surgery, that attract patients from a wider geographic area. Developing outpatient services and telehealth options can also improve access and generate revenue.
- Strategic Partnerships and Alliances: Collaborating with other healthcare providers, such as physician groups, accountable care organizations (ACOs), and other hospitals, can create economies of scale and improve efficiency. These partnerships can facilitate the sharing of resources, reduce duplication of services, and improve care coordination.
- Advocacy: Actively advocating for policies that support non-profit hospitals and protect access to care is crucial. This involves working with policymakers at the local, state, and federal levels to ensure adequate funding for government programs and fair reimbursement rates.
The survival of non-profit hospitals is essential for maintaining a strong and equitable healthcare system. Their commitment to providing care to all, regardless of ability to pay, makes them a vital safety net for vulnerable populations. By diversifying their funding streams, implementing effective management strategies, and advocating for supportive policies, non-profit hospitals can navigate the challenges of the healthcare landscape and continue to serve their communities for generations to come. The challenges are significant, requiring ongoing adaptation and innovation, but the critical role these institutions play in our society necessitates a concerted effort to ensure their long-term viability.